Over the past 2 decades, 3D-printing has emerged as an exciting and powerful technological advancement in various medical fields. This rapidly evolving field of study has enabled researchers to fabricate previously impossible materials into specialized shapes and forms. In tissue engineering, 3D-printing offers a great deal of control and the ability to create complex architectures for use as tissue scaffolds. Scientists conducting laboratory research have found that this new implant technology can promote a cellular response and initiate bone healing. In orthopaedics, implant technology is changing the way surgeons are treating patients with musculoskeletal disorders and injuries, in particular, those affecting the cervical spine (neck).
Spinal Implants
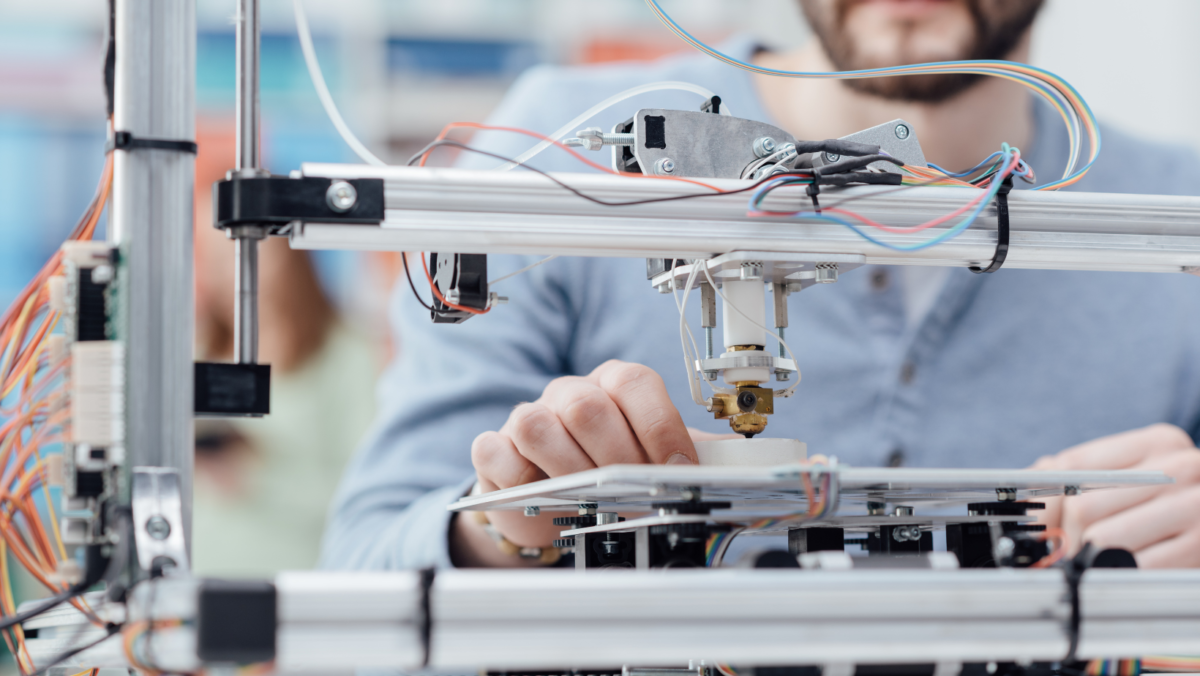
Laboratory data have demonstrated that 3D computer printing can produce spinal implant materials that have bioactive properties, which can enhance the regenerative process. For example, researchers have designed spinal spacers with a porous structure that signals nearby cells to grow bone and allow bone cells to grow into and through the spacer implant (Fig. 1). In early clinical studies, 3D-printed spacers have demonstrated improved fusion and better clinical outcomes compared to spacers made of plastic or metal.
Physicians treat most degenerative conditions of the cervical spine successfully by nonoperative means involving therapy and medications. However, progressive neurologic deficits with persistent, painful symptoms lasting more than 6 to 8 weeks are often indications for surgical treatment (Fig. 2). For example, stenosis (narrowing) of the spinal canal can cause chronic pain, numbness, and muscle weakness in the arms or legs. To resolve these symptoms, a spine surgeon can perform a laminectomy (decompression surgery) by taking out a small piece of the vertebrae, called the lamina, and by removing any disc fragments or bone spurs that have applied pressure to the spinal cord or nerves. The goals of the surgery are to enlarge the spinal canal for the spinal cord and nerves to pass, to re-establish normal disc space height, and to improve spine curvature. The surgeon may also perform an interbody fusion during the cervical decompression to provide permanent stabilization of lordosis (curvature) and disc space height. A successful clinical outcome is achievement of a solid fusion between the 2 vertebrae.
Spinal fusion
A spinal fusion is a surgical process that involves creating new bone formation across a spinal disc space (Fig. 3). Fusion in the spine is a complex process and the disc space is a challenging healing environment. In spinal fusions, interbody spacers are used in the disc space to unite 2 vertebrae together. The spacers serve a variety of purposes; they provide fixation, preserve the height of the disc space achieved during surgery, and encourage the bone graft to grow from one vertebral body into to the adjacent vertebral body. Surgeons use a bone graft to support the fusion process and provide elements to support bone growth. This fusion process is a race between resorption of the graft material and the formation of new bone, which grows through the graft to connect the 2 vertebral bodies. A successful interbody fusion induces new bone formation that bridges the disc space in order to help support viable bone.
Surgeons are using state-of-the-art 3D-printed spacers to attempt to win the race between resorption and the formation of new bone. Some research studies and case reports of patients who have undergone anterior cervical discectomy and fusion using an FDA-approved 3D-printed spacer device have reported good outcomes. Following surgery, the patients reported improved neurologic function, less pain, and improved physical outcomes, and at 3 months following surgery, radiographs demonstrated fusion progress across each disc space with bony ingrowth. Additionally, there were no instances of hardware failure or migration of the implant. Spinal alignment was similarly improved and maintained.
Good results
Although 3D-printing is still in the early stages of development for cervical implant surgery, the safety and efficacy of the technology is steadily emerging. One benefit researchers are finding comes from using the patient’s anatomy to design the device. Since the device is custom-made, surgeons are able to preserve anatomy by removing less surrounding structures. Preserving anatomy can lead to shorter operative times, a better fit of the implant, and improved stability. The research thus far suggests that in the treatment of degenerative disc disease, unique 3D-printed interbody devices are safe and present a suitable alternative for successful outcomes in anterior cervical spine surgery.
Author: Matthew McGinty, BS and Sohrab Vatsia, MD | Columbus, Georgia
Last edited on November 29, 2023