In the very early days of spine surgery, the surgeon had little more than his or her training, experience, and a scalpel to perform complex and delicate musculoskeletal cases. The traditional surgery was often “invasive,” meaning that the procedure required a sizeable incision, and cutting into muscles to reach the problem area. With damage to the soft tissue, it often took patients months to heal and to return to normal activity. Although the approach to back surgery was invasive and required a long recovery, it was the only option for many people seeking relief from chronic back pain caused by ruptured discs, trauma, tumors, deformities, degenerative disc disease, and infection. Surgeons perform minimally invasive procedures through tiny incisions instead of a large opening. These procedures, both diagnostic (an exam or test to determine a condition, disease, or illness) and therapeutic (a treatment), have been around for a long time. In 1939, orthopedic surgeons first performed knee arthroscopy. Since then, minimally invasive procedures have advanced significantly, becoming the mainstay across orthopedics.
 Minimally invasive spinal surgery
Minimally invasive spinal surgery
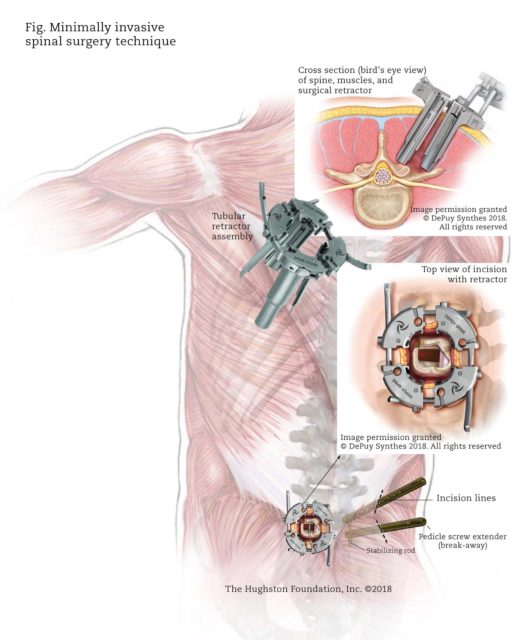
With traditional open spinal surgery, the surgeon makes a long incision and then retracts, or moves the muscles to the side. Once the muscles are moved, the surgeon can access the spine and remove any diseased or damaged bone or tissue. Then, the surgeon can place bone graft material, cages, rods, or screws as needed. In contrast, the surgeon who practice minimally invasive spinal techniques use tiny incisions and special instruments to perform the surgery (Fig).
Researchers developed less invasive surgical techniques to treat spinal problems with less injury to the muscles and other structures in the spine. Those who perform this specialized surgery are spinal surgeons with additional training in minimally invasive surgery. There are a number of devices and approaches that help the surgeon perform spine surgery. For example, a major drawback of open surgery was the retraction of the muscle, which often caused damage to the soft tissue, resulting in additional pain and healing time. This problem has considerably improved with the use of the tubular retractor.
To do the surgery, the surgeon will make small incisions to reduce blood loss and limit tissue damage, and will use specialized tools and tubular retractors to separate the muscles while performing the operation. The tubular retractor holds the muscles open creating a tunnel to the problem area in the spine. The surgeon accesses the spine using small instruments that fit inside the tubular retractor. Bone or disc material can be removed through the retractor, and the instruments needed for the treatment, such as screws or rods are inserted through the tubular retractor as well. Some surgeries may require more than one retractor. Additionally, fluoroscopy (x-ray that shows real-time moving images) is used as a navigation system to help the surgeon pinpoint the problem with great precision. Fluoroscopy verifies the location of bones, surgical instruments, and implants, as well as soft tissues, such as organs and muscle. Using this technique, the surgeon can perform complex cases in less time and with fewer complications. Collectively, these tools and the skill of a qualified surgeon can successfully treat patients who have various herniated discs, bone spurs, tumors, or other tissues adversely affecting the spine. If the patient needs a spinal fusion, the same tools assist the surgeon in placing rods and screws in place to stabilize the spine.
The benefits
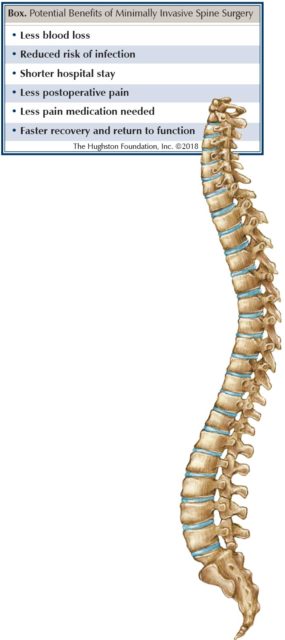
Patients who undergo minimally invasive spinal fusions typically experience less blood loss, less postoperative pain, a decreased hospital stay, and a faster return to function (Box). Additionally, postoperative infections seem to occur less often after minimally invasive surgery. Furthermore, most patients can walk on the day of surgery with physical therapy assistance and are typically discharged home the following morning. Patients also tend to need less pain medication and are able to return to the workplace sooner. Moreover, postoperative bracing is much less common, since the patient’s own internal brace—his or her own muscles—have been spared.
Is it right for you?
Spine surgery is not the first option for treatment of back pain. Physicians typically recommend spine surgery if the exact source of pain can be pinpointed and all other nonsurgical treatments have failed. Nonsurgical care, sometimes called conservative treatments, such as medications, rest, activity modification, and physical therapy should be attempted first, but if these fail to ease the pain, spine surgery may be recommended.
Each patient’s condition is unique; therefore, not everyone is a candidate for the minimally invasive approach. Physicians tailor medical treatments to fit each individual based on the patient’s diagnosis, overall health, and for those with limiting factors, such as obesity. In these situations, it may be medically advantageous or necessary to perform a traditional open surgery. Ultimately, the goal is to provide back pain relief and the best possible clinical outcome for the patient. While all surgery has its risks, back surgery today has benefited greatly from the advances in medical technology that now make many of our spinal surgeries minimally invasive. When looking into the future of spine surgery, surgeons feel that the advancements in technology will continue, which means better outcomes for patients.
Author: Todd C. Bonvallet, MD | Columbus, Georgia
Last edited on October 18, 2021