Contributing physicians in this story

 Technology is an ever-evolving part of our world. It seems to be integrated into almost every facet of our life—from cell phones, to travel, to our abilities to work from home, and of course, in our healthcare. Orthopaedics seems to be at the forefront as revolutionary leaps forward continue to fuel the advancement of medicine. The incredible progress visible to even the most untrained eye is astounding when it comes to knee replacement surgery.
Technology is an ever-evolving part of our world. It seems to be integrated into almost every facet of our life—from cell phones, to travel, to our abilities to work from home, and of course, in our healthcare. Orthopaedics seems to be at the forefront as revolutionary leaps forward continue to fuel the advancement of medicine. The incredible progress visible to even the most untrained eye is astounding when it comes to knee replacement surgery.
A German surgeon, who inserted a hinged-iron joint in 1860, performed the first version of a total knee replacement. That first procedure initiated an evolution of knee replacements, and in the 160-year span, the procedure has undergone numerous reiterations with constant improvement. Nevertheless, it seems that just recently, the ability to incorporate computers and robotics has proven its worth.
What is robotic-assisted surgery?
Now when we speak of robotic knee replacement, we need to clear up the actual verbiage. More appropriately, it is a robotic-assisted knee replacement. This simply means that the robot is a tool that surgeons can use to perform a more precise and reproducible surgical procedure. The robot CANNOT and WILL NOT do the surgery without the surgeon. The surgeon is still entirely responsible for the patient and the procedure. In fact, the first 10 minutes or so in the operating room is routine exposure performed by the surgeon and assistants without the robot at bedside. However, once the time comes, the robot then provides invaluable information and technology to help the surgeon perform the procedure.
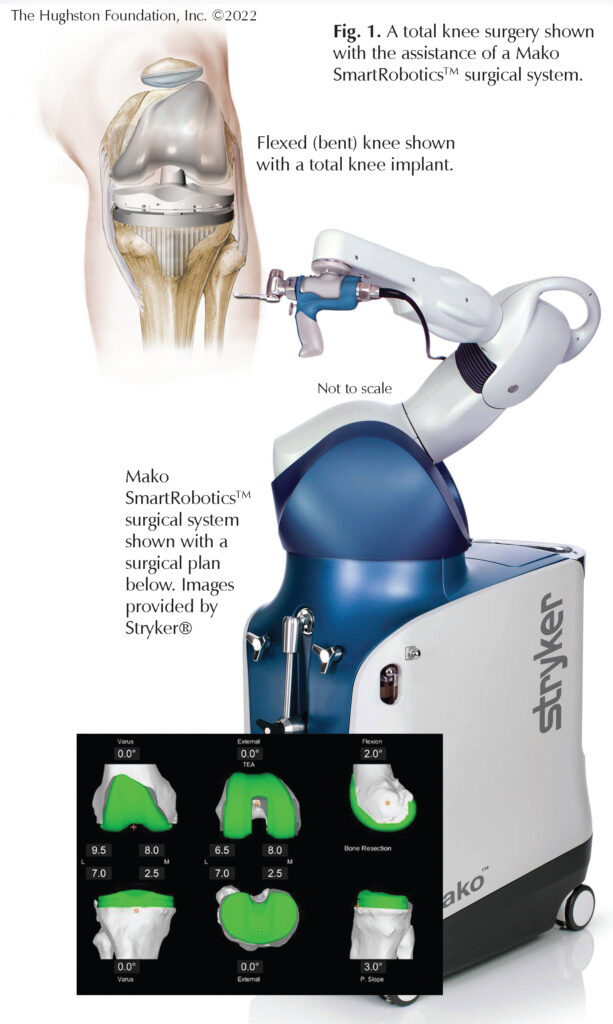
There are several different variations of robots available for assisting surgeons in total knee replacements. These range from passive systems, which provide information to the surgical team without assisting in the technical aspects of the case; active systems, which have the ability to perform tasks autonomously; and semi-active systems, which actively participate in the surgical procedure with the guidance of the surgeon in charge. My personal experience and preference is using the Mako Smartrobotics™ surgical system, which is in the category of robotic-arm-assisted technology. This system has been in use since 2005. It plays a role in hip replacements, partial knee replacements, and total knee replacements.
In order for a surgeon to be eligible to incorporate this skill into their practice, there is additional required training followed by proctored cases by a Mako Smartrobotics™ certified surgeon. Once integrated into a surgeon’s practice, there is a misconception that there may be additional fees or time associated with the procedure. Typically, the use of a robotic system does not incur any additional cost to the patient or their insurance. The robotic assistance has actually improved surgical times by helping to ensure more precise implant position the first time with a dramatically lower rate of needing alterations in cuts. This is likely due to the incredibly accurate planning the system performs prior to initiating any bone cuts.
Why do surgeons perform robotic-assisted surgery?
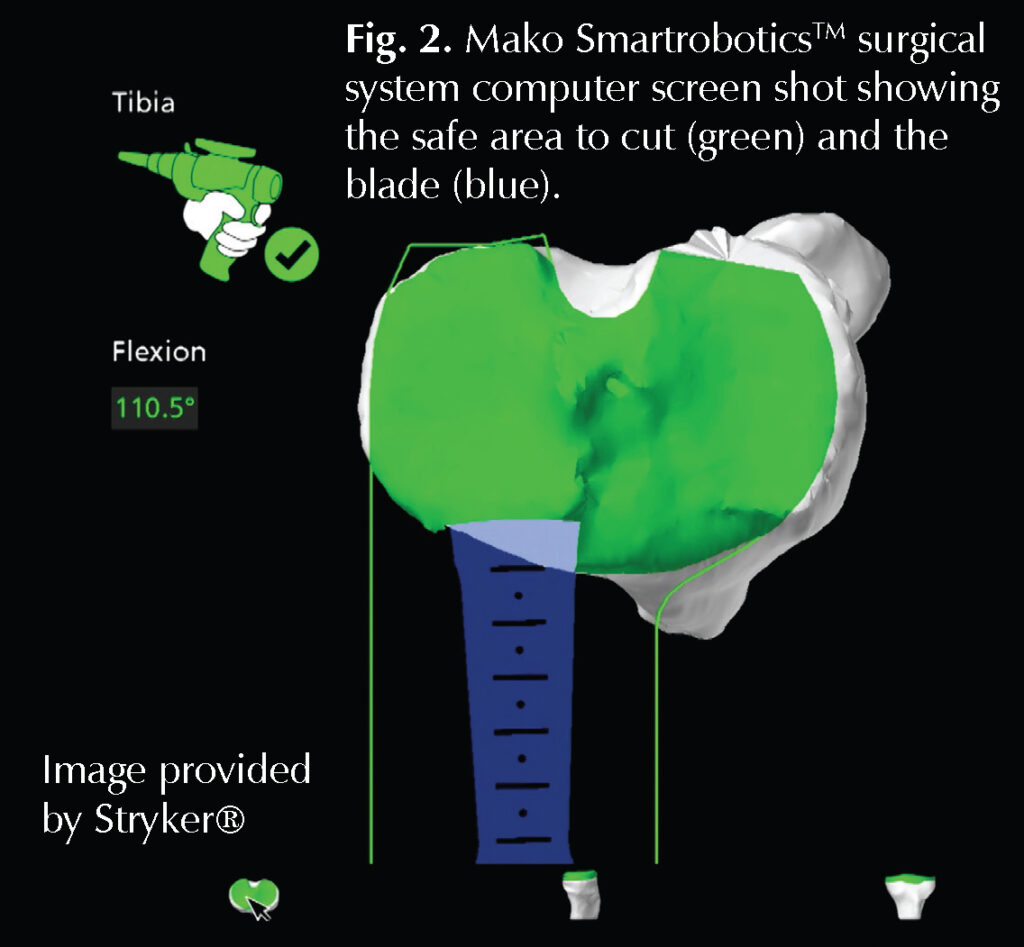
So why would a surgeon change their practice and do more than the required training for a surgery that does not make any more money? I have personally participated in hundreds of knee replacements during my training using a tried and true traditional method. A method that does not rely on robotics, was very reproducible, and has good outcomes. However, once I established my own practice in Tennessee, I obtained Mako Smartrobotics™ training for numerous, well-considered reasons. First, this procedure has a growing body of publications supporting its effectiveness. The Mako Smartrobotics™ has the ability to improve accuracy and reproducibility in terms of bone cuts and implant placement. Ideally, with long-term data we hope to see this translate to better survivorship. A unique feature of the robotic-assisted technology robotic system is that it has protective boundaries. This means that while the surgeon is using the robot to very precisely complete bone cuts—accurate within 1 mm of planned—the saw which is held by the surgeon, but attached to the robotic arm, does not allow cutting outside of the preplanned area (Fig. 2). This advantage decreases the risk of injury to surrounding soft tissues, such as the vital posterior neurovascular (nerves and blood vessels) structures when compared to nonrobotic surgery. There is also some evidence showing decreased postoperative pain and improved patient satisfaction scores with Mako Smartrobotics™ assisted knee replacement when compared with traditional, nonrobotic knee replacements.
Talking with my doctor
There are many ways to address knee arthritis; therefore, surgery is chosen once other treatment options no longer provide satisfactory relief. I also advocate that bad x-rays alone are never a reason to proceed with a knee replacement. Surgeons are not in the business of treating x-rays. Instead, we treat the person, not the picture. Once the doctor makes a diagnosis of arthritis, the severity of symptoms outweigh the severity of x-ray findings. The decision for a knee replacement should be made once a patient is personally, professionally, medically, and mentally ready to undergo this surgery. After the decision for surgery is made, we acquire insurance authorization, which is typically not an issue and no more difficult to obtain than if performing a traditional knee replacement.
How is the procedure performed?
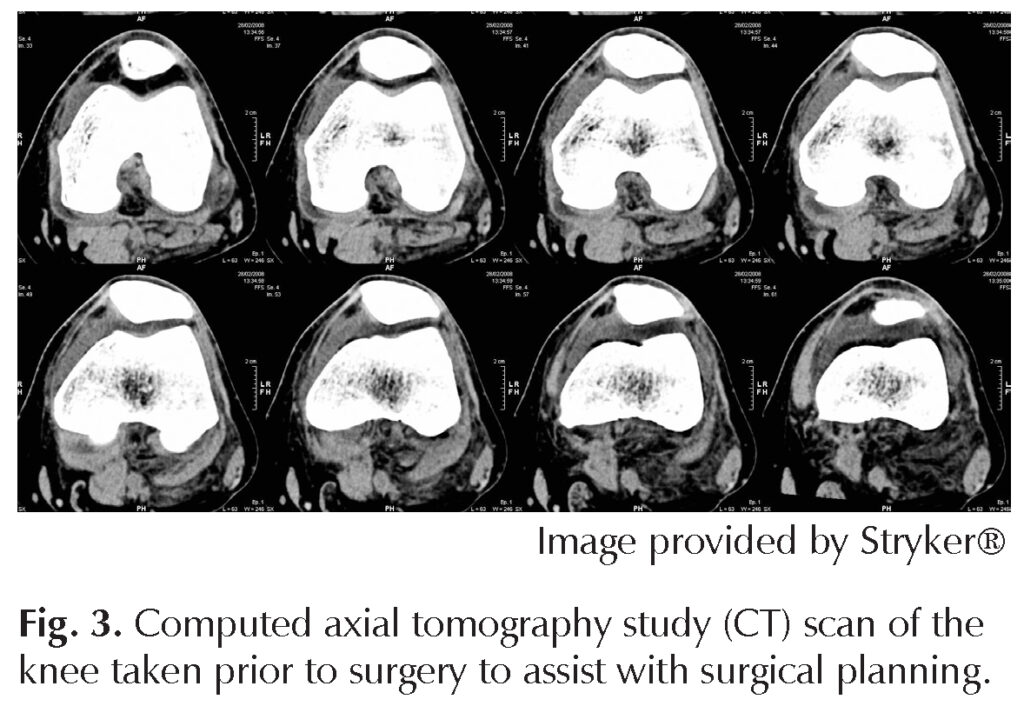
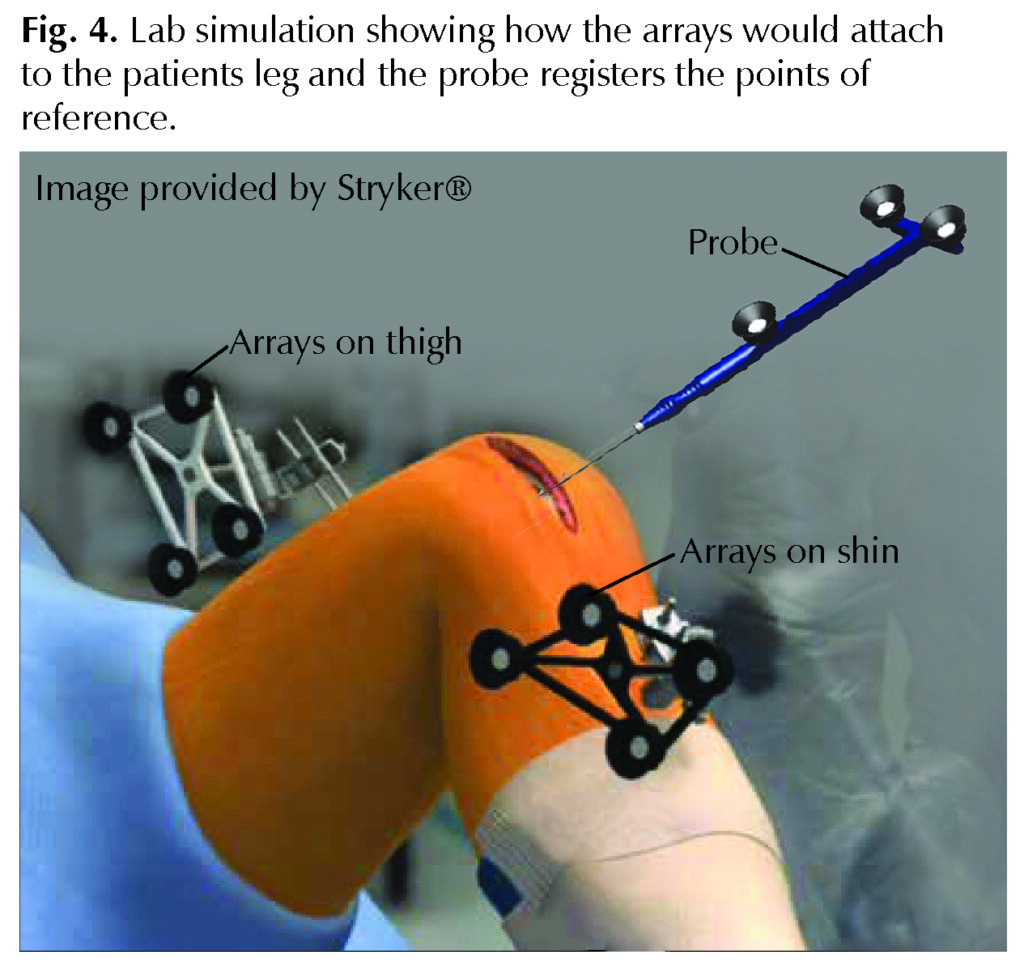
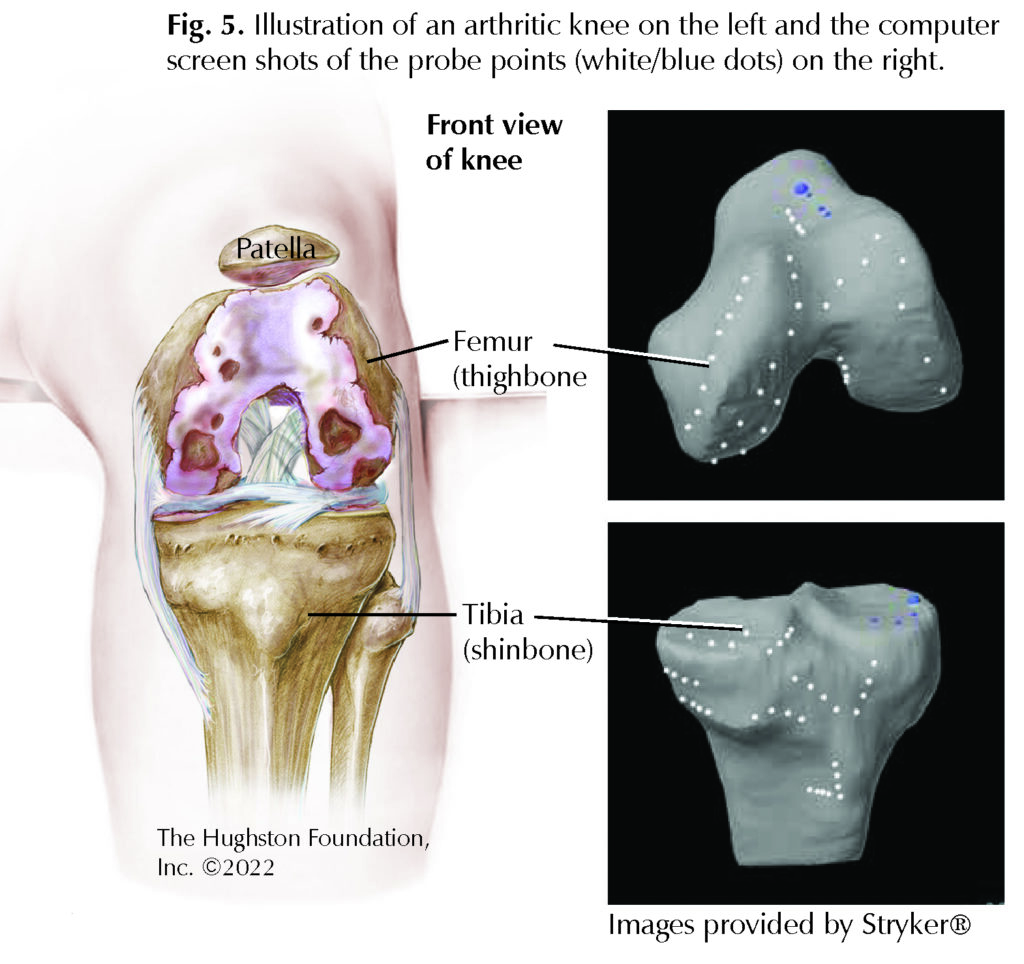
Preoperatively, the patient obtains a computed axial tomography study (CT) scan from hip to ankle, which includes the knee (Fig. 3). The scan provides a 3D reconstruction of the knee itself for planning purposes and it determines the perfect mechanical axis—an imaginary line that lies between the center of the hip to the center of the ankle, and which the center of the knee passes through. This is the basis of establishing robotic-assisted knee replacement surgical planning. Then, once the patient is in the operating room, the surgeons makes the routine exposure and surgical approach to the knee. Then the surgeon attaches arrays to the patient’s leg (Fig. 4). Arrays are small reflective disks that the robot can closely track to follow leg position. Next, is registration where dozens of points within the exposed knee are touched with a special probe in order to correlate the anatomy found intra-operatively with the CT findings so that the robot now knows precisely how and where the knee is located (Fig. 5). Now, the surgeon removes any large bone spurs and manipulates the knee to as close to straight as possible. The Mako Smartrobotics™ system can now formulate the planned cuts (Fig. 6 – next page). The surgical team brings in the robotic arm and the surgeon uses a saw attached to the robotic arm to make incredibly precise cuts (Fig. 2). Once cuts are complete, the remainder of the tissues are prepared, the surgeon inserts the new knee components, and the wound is closed.
After surgery
Physical therapy begins as soon as possible. The patient may fully bear weight and immediately move the knee. Most patients can return home the same day as surgery. Although the surgical technique is obviously important, the postoperative therapy and hard work by the patient is equally as important. Physicians encourage therapy early and often, because most of the motion that a patient obtains for the remainder of their life is gained in the first 8 weeks after surgery. Although full weightbearing and motion is permitted immediately after surgery, often patients ambulate with a walker for about 2 weeks and then transition to a cane for an additional few weeks.
My recommendation
I have been using robotic-assisted technology for almost 9 years and I do not foresee myself ever returning to traditional methods. In my opinion, it has afforded me the opportunity to do a better surgery in less time with a better recovery for my patients. Due to our experience with this technology, we have patients from many distant regions traveling for this technology and our expertise with it.
Something I strongly suggest to every patient is to ask their surgeon, “What would you do if it were your family?” Well, my own father and aunt have driven over 5 hours to have their knee surgeries completed as outpatients using the Mako Smartrobotics™ upon my recommendation. Therefore, I am happy to advocate the same to all patients willing to consider this advanced technology for their impending knee replacements.
Author: Lucas B. Richie, MD | Nashville, Tennessee
Last edited on December 22, 2022