Contributing physicians in this story
Arthritis and rheumatic conditions are a leading cause of disability among adults in the United States. Almost 50% of Americans, 65-years-old and older have been diagnosed with arthritis. As baby boomers age, the number of people who will need treatment for knee and hip arthritis is expected to skyrocket. Many will consider total knee and total hip arthroplasty (joint replacement) to alleviate their symptoms.
Over the years, orthopedic surgeons have refined the surgical approaches used in knee and hip arthroplasty. The goal of the surgical approach is to gain enough exposure (allows access and visualization of the bone) to complete the surgery while minimizing the effects to the surrounding tissues. Improvements in both technique and instruments have allowed us to minimize injury to the muscles and tendons (connects muscles to bones). With a trend towards shorter hospital stays, and even outpatient surgery, we continue to look for new ways to speed recovery after surgery.
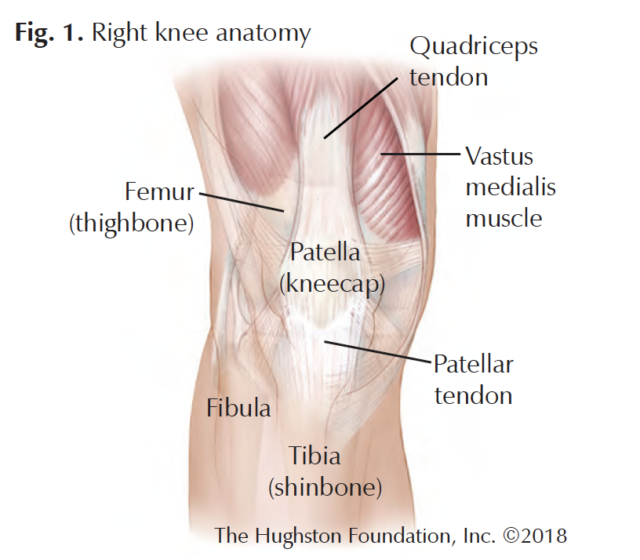
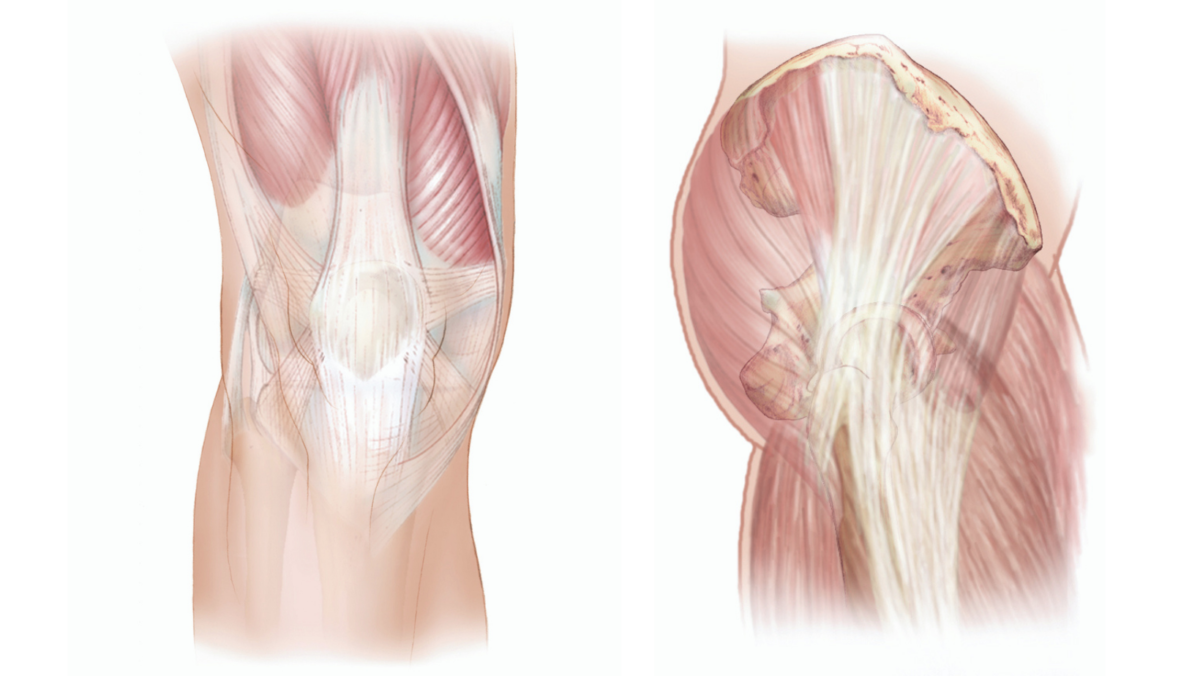
Each surgical approach has its advantages and disadvantages; but how your surgeon performs your surgery often depends on his or her own preference, your overall health, and health history (Figs. 1, 2 & 3). For example, if you have arthritis, if you are thin or obese, if you have damaged your knee or hip joint in the past, or if you smoke—your surgeon considers all of these factors and more before surgery.
Surgical approaches to the knee
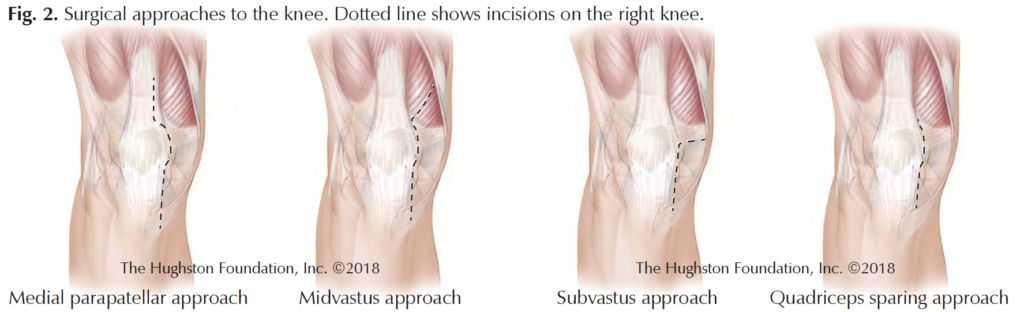
Medial parapatellar approach
For many years, this approach has been the standard incision for orthopedic surgeons. The medial parapatellar incision descends down and around the patella (kneecap), offering the best view of the joint. The disadvantages, however, include cutting into the quadriceps tendon, which then requires repairing, and during the procedure the patella is flipped over, sometimes stretching the knee tendons in the process.
Midvastus approach
First described by Gerald A. Engh, MD, and colleagues in 1997, the midvastus approach is a variation of the medial parapatellar approach that does not cut the quadriceps tendon. Instead, this incision splits the vastus medialis muscle and requires repair and healing of the muscle fibers. Depending on the surgeon, the patella may be flipped during this approach.
Subvastus approach
The subvastus approach, which is a L-shaped incision below the vastus medialis muscle actually elevates the muscle instead of cutting into it and this procedure also avoids flipping the patella. A drawback, however, is that patients who are obese, or who have limited range of motion may not be good candidates for this approach. Additionally, since the surgeon elevates the muscle, this approach may be difficult for patients who are muscular with a large vastus medialis muscle.
Quadriceps sparing approach
This is the most minimally invasive approach since it completely preserves the quadriceps tendon and its muscle attachments and there is less tendon stretching since the kneecap is not flipped. The disadvantages are that it provides the least exposure for the surgeon and some studies have demonstrated an increased complication rate.
Surgical approaches to the hip
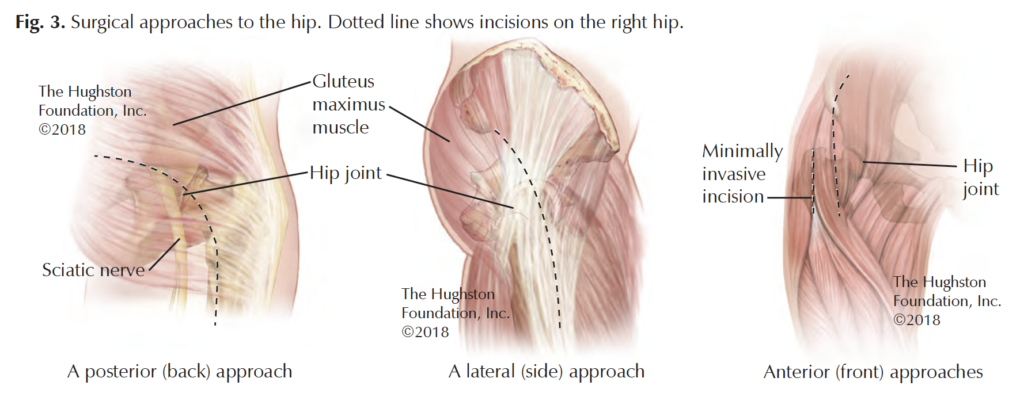
Posterior approach
The posterior (back) approach is the most common surgical approach used for total hip replacement worldwide. Surgeons perform this procedure with the patient lying on their side. The posterior approach involves splitting the gluteus maximus muscle in line with the muscle fibers and the short external rotator muscles (muscles that allow outward rotation of the hip) are detached either completely or partially and then repaired at the end of the surgery. Surgeons prefer this approach because it offers an extensile (stretched or open) exposure that provides an excellent view of the femur (thighbone). The disadvantages include a slightly higher dislocation (comes out of socket) rate and a muscle-splitting approach.
Direct lateral approach
The modern direct lateral (side) approach was popularized by orthopedic surgeon, Kevin Hardinge in 1982. It is the second most common surgical approach for total hip arthroplasty used worldwide. Surgeons perform the surgery with the patient on either the side or supine (face up). Similar to the posterior approach, the direct lateral approach involves splitting the gluteus maximus muscle and a portion of the gluteus medius muscle (muscle that stabilizes the hip while standing) for good exposure for the surgeon. Advantages of the direct lateral approach include the lowest dislocation rate among the most popular approaches and an excellent view of the acetabulum (socket). The major disadvantages of this approach are a significant incidence of limp and abductor (movement away from the body) muscle weakness.
Direct anterior approach
Dr. Marcus Smith–Petersen first described the anterior approach to the hip in 1917, when physicians primarily used it for reducing congenital (at birth) hip dislocations. In recent years, this approach has regained popularity with modifications to the original procedure and the development of new instruments specifically used for anterior hip arthroplasty. It is now the third most common surgical approach used for total hip replacement worldwide. This approach is truly intermuscular and internervous. In other words, surgeons do not cut or split major muscles and they navigate between nerves. The advantages of the direct anterior approach are a low dislocation rate with a muscle-sparing approach, which means faster soft-tissue healing. The disadvantages of this approach are a lack of exposure of the femur and some studies have suggested an increased fracture risk.
Newer approaches
More recently, surgeons have developed the supercapsular percutaneously-assisted total hip, or SuperPATH approach and the direct superior approach. Both of these approaches are variations of the posterior approach, but with smaller incisions and less soft tissue damage that are meant to improve postoperative recovery. The SuperPATH also avoids dislocation of the hip during the procedure.
Which is the right approach?
Surgeons have successfully performed knee and hip arthroplasty using a variety of approaches for many years now and these surgeries have been tremendously successful for treating patients with disabling arthritis. Each surgical approach has advantages and disadvantages and the scientific evidence has not demonstrated a superior approach for any procedure. When considering surgery, the patient’s overall health and lifestyle, along with the surgeon’s experience are paramount in making the best decision on the approach to use.
Author: Randall J. Ruark, MD |Columbus, Georgia
Volume 30, Number 1, Winter 2018
Last edited on October 18, 2021