Wide-awake local anesthesia with no tourniquet, or WALANT, is an anesthetic technique used by surgeons to achieve pain control at the operative site through a local injection. Most surgeons use WALANT in the upper extremity for cases such as trigger finger release, carpal tunnel release, flexor tendon repairs, and fracture care; however, the technique is gaining popularity for other areas, including trauma and foot and ankle surgery (Table 1).
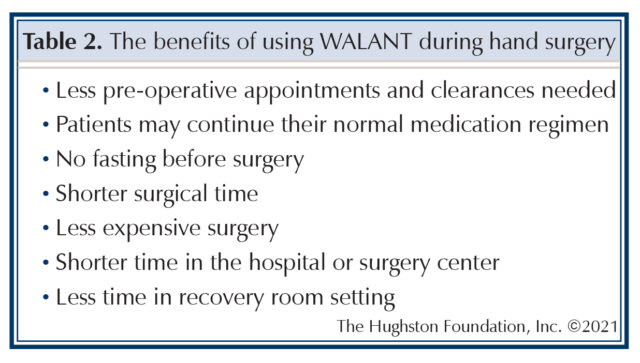
Dr. Donald H. Lalonde first described using wide-awake local anesthesia with no tourniquet in treating operative hand cases. Since its introduction, WALANT has continued to gain popularity among surgeons with high patient satisfaction and clinical outcomes. This anesthetic technique allows patients to be awake during their surgical procedure without pain from a tourniquet (Table 2). Another added benefit, is the ability for the patient to participate by moving their extremity as indicated by the surgeon depending on the surgical procedure. In addition, no intravenous, or IV (within a vein) is required and the patient does not have to undergo formal sedation. The use of WALANT also provides a potential cost saving benefit to the healthcare system by decreased operative times, avoiding pre-operative clearances for general anesthesia, and decreased use of hospital resources.
Steps for an effective WALANT procedure
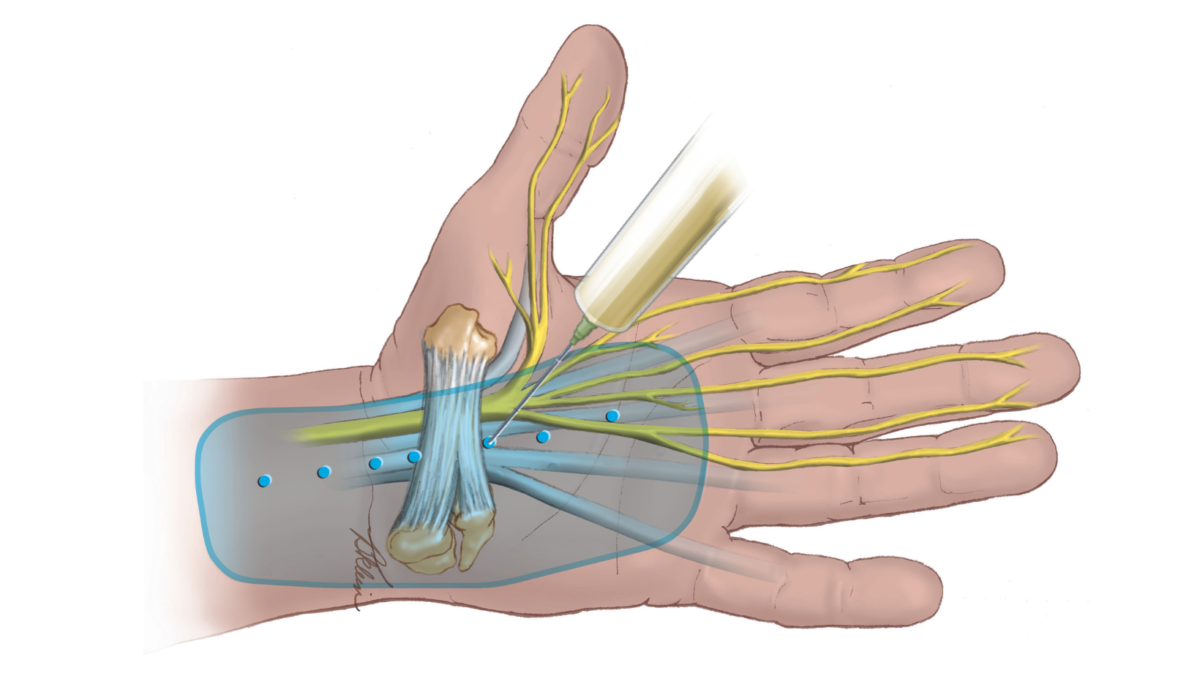
The surgeon sees the patient in the pre-operative waiting area, marks their surgical site, and explains the procedure in detail. Typical injections include a mixture of room temperature lidocaine, which blocks pain, and epinephrine, which stops bleeding, and sodium bicarbonate, which buffers the solution to make it less painful. The size of the needle used is typically a 27 or 30-gauge needle. The physician presses firmly on the injection site to help decrease the initial needle stick the patient will feel. The surgeon stabilizes the syringe with the injection using both hands and slowly injects a small amount under the skin. The doctor then asks the patient to say when the pain has stopped from the initial needle stick. At that time, the physician slowly injects the local anesthetic. Ideally, the patient will only feel the first needle stick. The surgeon continues to inject the operative site with the anesthetic mixture to ensure you gain the full anesthesia effect.
Can I feel anything during a WALANT procedure?
You will feel the initial needle poke that is no worse than an IV stick, which is what you would otherwise feel if you have surgery under an anesthetic. You may be able to feel that the surgeon is doing something, but you do not feel anything painful. What you can do is move your hand, if instructed to do so by your surgeon, or you can listen as the surgeon tells you what he or she is doing. You can bring headphones to listen to music or watch a video to distract yourself if you believe this awareness may bother you.
Are there any complications or side effects during surgery?
There are 2 common problems that can occur after lidocaine and epinephrine injections, but both of these can be overcome. The first is nervous jitters or trembling that can occur after an epinephrine injection. You may feel a little jittery or shaky after the injection, which is similar to the feeling after consuming too much coffee. Physicians consider this a normal reaction to the adrenaline in the numbing medication that will go away after approximately 20 to 30 minutes.
The second common problem is a vasovagal syncope episode that can make you feel dizzy, nauseated, or sweaty. After the injection, some patients may begin to feel faint because their body overreacts to certain triggers, such as the sight of blood or extreme emotional distress. The vasovagal syncope trigger causes your heart rate and blood pressure to drop, but this is typically not a severe health condition. Some people have a similar reaction when they donate blood. A vasovagal response can be limited by having the patient lying down instead of sitting up. However, even if lying down, some patients may complain that they are not feeling well or that they are going to be sick. They may also get pale or show signs of imminent fainting. If you begin to feel faint, the nurse may reposition your bed to where your head is lower than your feet. Often, with these measures, most patients usually begin to feel better within minutes. While both of these side effects result after the injection, they are not an allergic reaction to the medicine.
What happens after my surgery with WALANT?
After surgery using WALANT, your nursing staff will take you to the postanesthesia care unit (PACU) where the surgeon can talk to you about the procedure and your postoperative care. Your surgeon will discuss your surgery and give you follow-up instructions. At that time, you can go home because you do not have to wait for the effects of general anesthesia or sedation to wear off. Your surgeon’s staff will schedule you to come back for your first follow-up appointment at postoperative day 10 to 14 depending on the surgical procedure.
What are the potential complications?
With the use of epinephrine, constriction of the blood vessels may occur leading to damage of the tissues, but many studies have shown this risk to be minimal. In the event of constriction, there are medications available to reverse these effects. Additionally, the use of epinephrine can cause an elevated heart rate in patients with cardiac conditions, but these risks are also minimal. Overall, the risk of complications from WALANT remains small, and with the benefits to the patient and healthcare system the usage continues to grow.
Am I a candidate for WALANT?
The use of WALANT provides many benefits; however, before making your decision, you should discuss the pros and cons of the technique with your surgeon. Patients with poor peripheral circulation, vascular conditions, or previous vascular injury should avoid WALANT. Patients with extensive heart or lung conditions should discuss further with their provider if they are a candidate for WALANT.
Your physician will take into account your desire for WALANT; however, some patients are better served having sedation. For example, patients with psychological disorders such as high anxiety or severe post-traumatic stress disorder may not tolerate a wide-awake procedure and may prefer to undergo other forms of anesthesia. Further, patients with allergies to the local mixture should also avoid WALANT.
You can flex for better outcomes
Active patient participation offers many advantages for the surgeon to evaluate the strength and function of the repair. Patients have the ability to perform the active range of motion, enabling surgeons to identify possible impingement or problems with implants. For example, by asking the patient to actively flex and extend the flexor tendon during a repair, the surgeon has the opportunity to vent pulleys, which may be prohibiting full range of motion in the finger. Your surgeon may find gaps in a repair before final closure that can prevent another rupture or injury. Additionally, visualizing the integrity of the repair in full active flexion and extension enables the surgeon to permit full or half flexion days after your procedure.
Over the past decade, the WALANT technique has proven to be valuable to both patients and surgeons by optimizing patient satisfaction and providing substantial healthcare savings. The advantages of WALANT offer patients the convenience of fewer office visits while avoiding the need to obtain pre-operative clearances and pre-surgery fasting. Some surgeons perform the procedures in an office setting while others use smaller surgical centers, with result in sizeable cost savings.
Author: Devin W. Collins, DO | Columbus, Georgia
Last edited on April 10, 2024