Contributing physicians in this story

The discipline of hand surgery has been around for a very long time with early contributions from such historic figures as the ancient Greek scholars Hippocrates and Galen. While hand surgery in America has evolved, since its formal recognition during World War II, advances in the tools and techniques used by hand surgeons continue to improve and help bring better surgical outcomes for patients.
Wrist fractures
Affecting both young and old, wrist fractures are some of the more common bony injuries seen in orthopedics. The injury often refers to a fracture of the end of the radius (larger forearm bone on the thumb side) (Fig. 1). The radius has a thin, hard (cortical) outer surface and a porous (cancellous) spongy internal composition, naturally making it weaker on the inside. For the elderly patient, the cancellous bone is often weak and in those with osteoporosis (a disease that causes thin, porous bone) it is even weaker still. Consequently, a fracture can occur with relatively minor trauma in this group of patients.
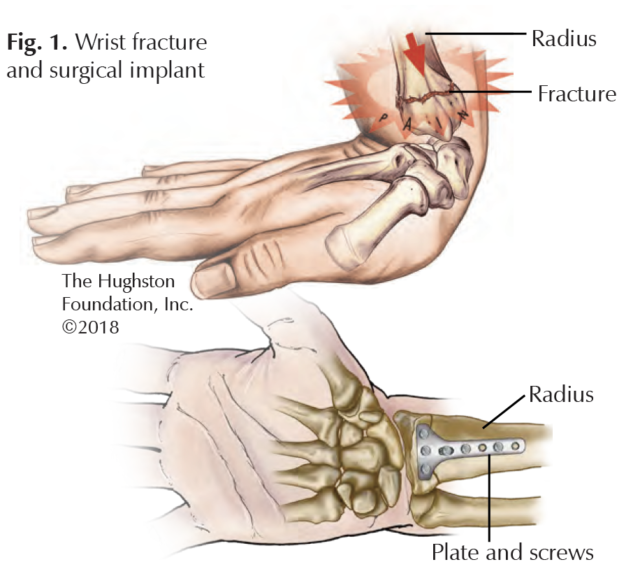
Historically, wrist fractures were treated with casting and nonsurgical methods. Attempts to intervene with surgery were often plagued by poor results and complications. This made the inherent risks outweigh the benefits of surgery in a substantial number of patients with severe fractures. However, the surgical treatment of wrist fractures improved dramatically with the introduction of locking-plate technology. This innovation allows stabilization of the distal radius, by using a plate and an array of screws or pins that secure to the plate. Therefore, it does not rely on the soft bone to secure the hardware. It allows placement of the plate on the palm side of the radius, which decreases the soft tissue complications and irritation that can occur with implant placement. Additionally, newer designs and materials have resulted in hardware that can be used on the back of the radius as well as the advent of smaller fragment-specific plates to fix common fractures of the distal radius. Patient outcomes have improved as a result of supporting these fractures while allowing for early motion during the healing phase of treatment.
Nerve injuries
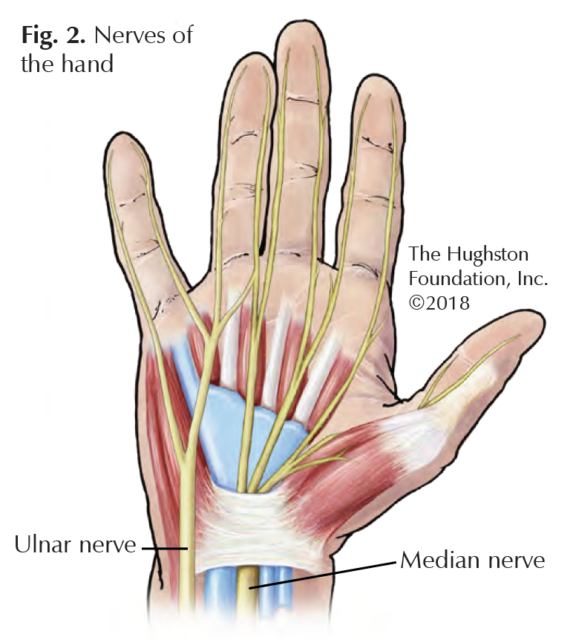
Nerve injuries have always been difficult to treat. The ability of a nerve to heal following injury is limited and the method of injury and timing are critical factors. Improvements in microsurgical techniques led to improved outcomes in nerve injuries of the hand and wrist, with prompt treatment being the key factor. The severed nerve starts to degenerate, or deteriorate following injury and over time becomes irreparable at the zone of the original injury. To stimulate nerve healing, the surgeon must cut away the scarred degenerative nerve tissue until reaching viable tissue. Healing depends on a tension-free repair and minimal distance between the nerve stumps at the site of injury. A significant gap makes this difficult and the results of surgery unpredictable (Fig. 2).
The use of a harvested vein conduit improved outcomes in nerve gaps less than 1 centimeter (cm) in length and the use of an autograft nerve (tissue taken from the patient) improved outcomes in nerve gaps in excess of 1 cm. Both of these techniques can result in persistent symptoms in the area of the harvested tissue. Recently, processed nerve conduits (artificial) and allograft (graft tissue from a donor) have led to improved outcomes without the negative issues related to harvesting tissue from the patient. The processed donor nerve tissue has shown promising results on larger nerve gaps with results similar to patient harvested nerves. This offers a variety of lengths and diameters providing a better match of the graft to the injured nerve in patients with severe nerve injuries.
 Carpal tunnel
Carpal tunnel
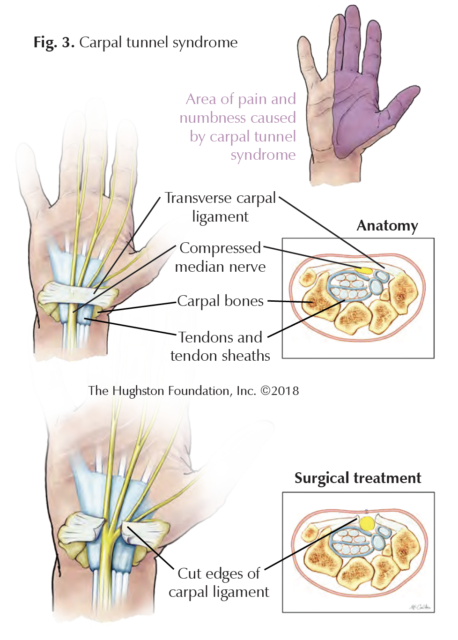
Carpal tunnel syndrome is pain, numbness, and weakness in the hand due to compression of the median nerve as it passes through a narrow passage on the palm side of the wrist (Fig. 3). Patient anatomy, medical issues, or repetitive activity can contribute to the progression of the syndrome. With symptoms occurring both day and night, the patient often complains of numbness in the fingers with the exception of the small finger. Patients report shaking their hand to try to resolve their discomfort and dropping objects held in that hand. Physicians diagnose the condition by obtaining a thorough medical history, a physical exam, and by obtaining a nerve conduction test. This nerve study measures how fast the electrical impulse moves through a nerve.
Managing the condition early with nonsurgical treatments includes observation, activity modification, nighttime bracing, and steroid injections. If these methods fail to control the patient’s symptoms, surgical decompression can provide relief of symptoms in most cases.
The surgery divides the transverse carpal ligament, thereby releasing the compression on the nerve, which allows it to recover. The ligament is a few centimeters long and attaches to bones in the wrist. Traditionally, the surgical incision could range from 4 or 5 cm up to 10+ cm in length and dissect the skin, subcutaneous fat, palmar fascia, muscle tissue, and then the ligament. Newer techniques now allow for less dissection and much smaller incisions. Mini-open techniques employing a 1 cm incision located at the wrist or in the palm have less dissection and disturbance of the overlying tissues while still accomplishing the desired ligament release.
Furthermore, researchers have developed endoscopic techniques that use smaller incisions and involve the placement of a camera underneath the ligament. This procedure allows the surgeon to release the ligament from below and it greatly minimizes unnecessary dissection of the soft tissue. A recent study comparing patients who had the endoscopic technique to those who had the traditional open surgery indicates that both groups received symptom relief and suffered similar postoperative aches and pains. However, the group who underwent endoscopic surgery had shorter surgical times, less scar tenderness, and experienced earlier return of grip and pinch strength. Mini-open and endoscopic techniques are innovations that have resulted in improved early outcomes for patients who undergo carpal tunnel surgery.
How far we have come…
Today, hand surgeons can use open, mini-open or endoscopic techniques and a range of tools, implants, and grafts to improve surgical outcomes for their patients. The techniques and tools have come a long way since the era of Hippocrates and Galen, which makes one wonder what they would think of our modern surgical methods.
Author: David H. MacDonald, DO, FAOAO | Columbus, Georgia
Last edited on October 18, 2021