
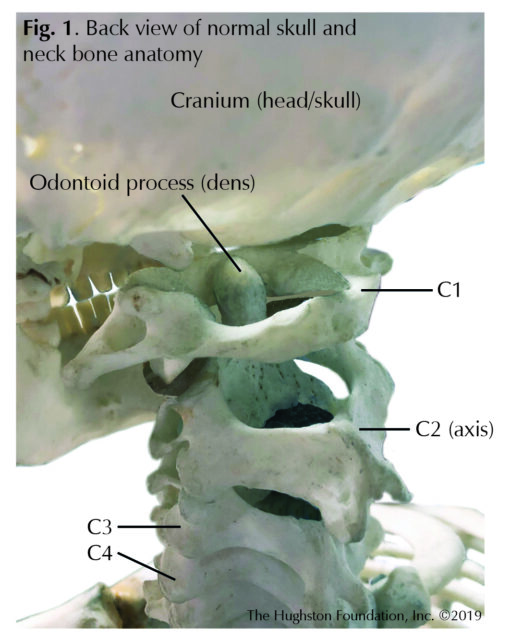
 The odontoid process is a unique peg-like bony structure of the C2 (second cervical) vertebra in the neck that physicians sometimes refer to as the dens (Fig. 1). Odontoid fractures can happen at any age, but the injury occurs most often in adolescents or older patients. In young people, the injury typically happens during a high-trauma event, such as a motor vehicle accident, but for older patients, it can occur during low-energy trauma, such as a fall. These fractures can alter the biomechanics (movement) of the cervical spine leading to pain, neurologic problems (numbness in the back, legs, and arms), and decreased stability. Sometimes these fractures are missed or left untreated, and they can be associated with increased morbidity (disease) in older patients. Overall, odontoid fractures are the most common fracture of the C2 vertebra and can account for up to 15% of all cervical spine (neck) fractures.
The odontoid process is a unique peg-like bony structure of the C2 (second cervical) vertebra in the neck that physicians sometimes refer to as the dens (Fig. 1). Odontoid fractures can happen at any age, but the injury occurs most often in adolescents or older patients. In young people, the injury typically happens during a high-trauma event, such as a motor vehicle accident, but for older patients, it can occur during low-energy trauma, such as a fall. These fractures can alter the biomechanics (movement) of the cervical spine leading to pain, neurologic problems (numbness in the back, legs, and arms), and decreased stability. Sometimes these fractures are missed or left untreated, and they can be associated with increased morbidity (disease) in older patients. Overall, odontoid fractures are the most common fracture of the C2 vertebra and can account for up to 15% of all cervical spine (neck) fractures.
Anatomy
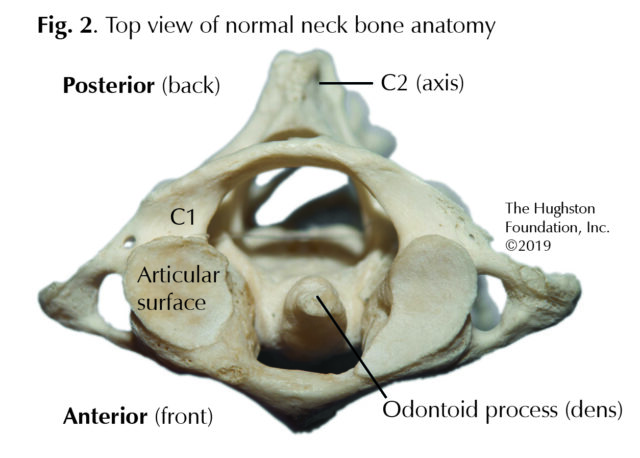
The second cervical vertebrae, also known as C2 or the axis, in the spine develops from a fusion process by the age of 12. At maturity, the C2 vertebra consists of the odontoid process and the body. The blood supply to C2 is from branches of the internal carotid artery (a main artery in your neck) and vertebral (spine) artery with limited blood supply in a portion of the odontoid, also known as a watershed area. The joint between C1 and C2 is unique in that it allows more movement than the other spinal joints. The dens is the size of your small finger tip, and it sticks up from the front of the C2 vertebra and fits into a groove in the C1 vertebra (Fig. 2). The odontoid process is the pivot for the C1 vertebra, which carries the cranium (head). Together C1 and C2 create the joint for side-to-side and up-and-down movement of the head.
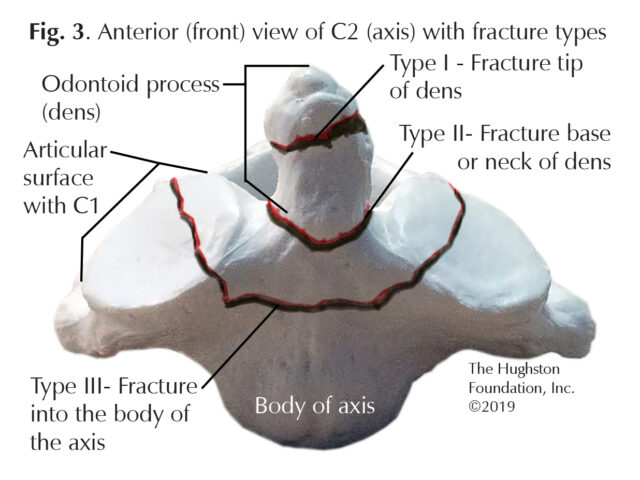
Classification of injury
Physicians use a 3-type classification system to diagnose and treat odontoid fractures (Fig. 3). With a Type I fracture, the tip of the dens is broken. Type I fractures are usually stable (does not move out of its normal position and alignment), causes pain, but does not create any neurologic problems, such as numbness in the back, legs, and arms. Type II fractures occur at the mid-portion (waist) of the odontoid and are known to have a high nonunion (a fracture that does not unite or heal) rate due to the watershed blood supply. Additionally, Type II fractures are often the least stable of the odontoid fractures; therefore physicians use further classification categories for Type II fractures (A, B, and C types). Type III fractures involve the lower portion of the C2 body at the C1 and C2 articulation.
An associated condition in the same region is an Os odontoideum (the dens fails to fuse to the rest of C2 during development), that may be mistaken as a fracture of the odontoid. This condition is typically benign and management consists of continued observation. There are differing opinions on the clinical importance of these findings; however, physicians believe they are due to an old trauma or from the odontoid not completely fusing during maturation.
Symptoms
Patients with odontoid fractures can present with a variety of symptoms. Often, patients complain of neck pain and stiffness that is exacerbated during neck movement. Difficulty swallowing, also known as dysphasia, is another common finding and can be associated with bleeding from the fracture site leading to a hematoma (blood collection). In rare instances, patients will have myelopathy (spinal cord injury) symptoms which may include abnormal reflexes, imbalance, and dexterity problems. Patients with neurological symptoms may complain of weakness in the hand and upper extremity and altered sensation.
Screening and diagnosis
When there is suspicion of an odontoid fracture, the first screening involves a series of radiographs. These x-rays include an anteroposterior (front to back) and lateral (side) view of the cervical spine. Physicians sometimes order a specific radiograph, known as the open-mouth odontoid view, to visualize the fracture. Additional radiographs may include cervical flexion (bending) and extension (straightening) views to assess for any instability. Advanced imaging can include a computed axial tomography study (CT scan uses x-ray and computer technology), CT angiogram (CT scan using injection of contrast material), or magnetic resonance imaging (MRI test that shows bones, muscles, tendons, and ligaments). A CT scan helps the clinician better visualize the fracture and assess for any instability. A CT angiogram allows the orthopedic surgeon to assess the location of vascular structures, including the vertebral artery. Localizing the anatomy and variations of the vertebral artery will be vital for surgical planning. The orthopaedist may order a MRI if neurologic symptoms are present and continue to persist, allowing the clinician to evaluate the spinal cord for damage and other soft tissue abnormalities.
Nonsurgical treatment
Orthopaedists determine management options depending on the severity of the fracture and other associated injuries and recommend either nonoperative or operative treatments. Observation and nonsurgical management may be ideal for patients with an Os odontoideum without instability or neurologic symptoms. Other nonoperative modalities include a hard cervical brace or halo vest immobilization. In general, physicians recommend these in stable odontoid fractures, in patients who are not surgical candidates, and in young patients with no risk factors for nonunion. Physicians usually prescribe hard cervical collars for most Type I fractures and often for Type II fractures in patients who are not able to have surgery. Additionally, physicians advocate using halo vest immobilization in Type II fractures in young patients without any risk factors that would predispose them to nonunions. Of note, halo vest immobilization is contraindicated (undesirable or improper treatment) in older patients because of high complication rates.
Surgical treatment
Orthopaedists recommend operative management for the majority of Type II and Type III odontoid fractures. Surgeons perform the surgery through different approaches including anterior (front), posterior (back), and transoral (mouth). Depending on the fracture pattern and associated injuries, the surgeon may perform a combination of these approaches to achieve the desired outcome.
Complications
With odontoid fractures, the most common complication and the most serious is a nonunion of the bones that can lead to an increased mortality rate. The risk factors include significant displacement of the bone, the angle of the fracture line, the spacing between the bones, and comminution (breaks in more than 2 pieces). Nonunions are more likely in Type II odontoid fractures, people older than 50, and those who delay treatment. Additionally, patients who use tobacco are at a higher risk for nonunions.
Rest assured
Odontoid fractures are not an uncommon injury of the cervical spine; therefore, you should seek care from an orthopaedic physician who specializes in the spine to ensure proper diagnosis and treatment. Every patient and odontoid fracture is unique, but rest assured that your orthopaedist will treat you with all variables in mind to obtain the best outcome.
Author: Devin Collins, DO | Columbus, Georgia
Last edited on July 27, 2022