
More and more young athletes are participating in a single competitive sport year-round instead of multiple sports through different seasons. This change in athletic competition has led to an increase in overuse injuries in the pediatric population. Sports medicine physicians often attribute the cause of these overuse injuries to a combination of an underdeveloped musculoskeletal system, increased duration and intensity of competition, and early sports specialization. One type of overuse injury that can have a detrimental impact on sports performance and the overall health of an adolescent athlete is a stress fracture.
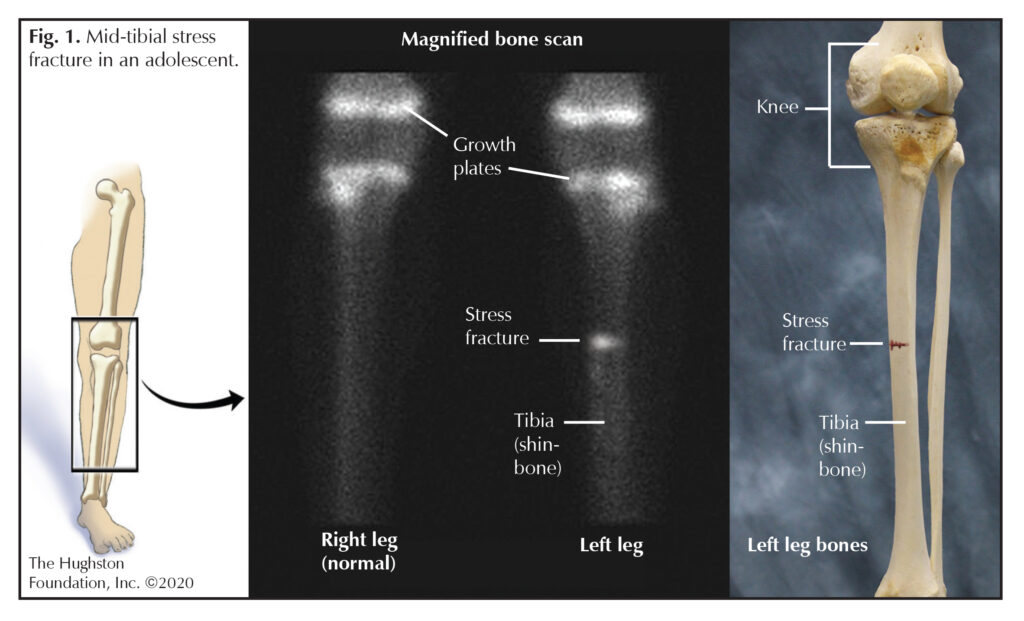
Stress fractures occur when abnormal stresses are placed on the trabecular bone (cancellous bone that is highly porous and located at the end of long bones) resulting in microfractures. Due to lack of adequate rest and recovery or underlying abnormalities in bone metabolism, these microfractures are unable to heal and remodel and can propagate over time. Continued repetitive loads exceeding the body’s normal intrinsic bone healing can eventually lead to complete fracture through the affected bone. The most common site for a stress fracture is the anterior tibia (shinbone) (Fig. 1), but the injury can also occur in the femoral shaft (straight part of the thighbone), femoral neck (below the ball of the hip joint) and posterior ribs (back ribs). Stress fractures can occur on the compression side (pushing together) or the tension side (pulling apart) of bones. Physicians can treat stress fractures on the compression side without surgery because the site is stable and has an adequate blood supply. However, stress fractures that occur on the tension side of a bone have poor healing potential and usually require surgical intervention.
Who is at risk?
Two major risk factors for the development of stress fractures are rapid increases in high intensity activity and abnormalities in normal bone metabolism. High intensity athletes as well as new military recruits are subject to rapid increase in training intensity especially during conditioning periods and basic training. Pediatric and adolescent muscles are underdeveloped and subsequently subject to early fatigue causing compensatory gait changes with increased stresses applied to the bone. This loss of the body’s ability to absorb shock from fatigued muscles combined with poor mechanics and improper training regimens can also cause overloading of these deconditioned muscles ultimately resulting in overuse injuries.
Ninety percent of a child’s bone mass is attained by the age of 18. Essential vitamins, such as vitamin D and calcium, play a vital role in a child’s developing skeleton. Athletes that are at risk of suboptimal bone mass and stress fractures include distance runners, gymnasts, and elite dancers. These sports require lean body mass and are often associated with disordered eating habits and irregular menstrual cycles in young female athletes. There has been a dramatic increase in the number of healthy children and adolescents who are at risk of vitamin D deficiency. Lifestyle changes that place children at risk for vitamin D deficiency include lack of outdoor activities, increased screen time, and poor diets. Inadequate oral intake of calcium and vitamin D, lack of outdoor physical activity, and abnormal estrogen levels can disrupt normal body homeostasis needed for appropriate bone growth and remodeling.
Symptoms, diagnosis, and treatment
Patients with lower extremity stress fractures most often present with complaints of pain in the anterior tibia, hip, or thigh that increases with running or physical activity. Over time pain can occur even with simple daily activities like walking or at rest. Symptoms usually develop insidiously and unrelated to a known injury.
Evaluation by a physician begins with a detailed history of symptoms and physical exam. The physician often orders radiographs (x-rays) which can demonstrate cortical thickening, or stress fracture. There may be signs on x-ray of bone healing, such as cloudy immature bone forming within 3 weeks of injury. If x-rays are negative, magnetic resonance imaging (MRI, a test that shows the bones, muscles, tendons, and ligaments) can help to evaluate the location of stress fractures as well as to assess the growth plate and surrounding soft tissues. A MRI can demonstrate subtle findings with exquisite detail of bone edema (fluid builds up as a response to injury) and fracture to confirm diagnosis without radiation exposure to the child.
First line treatment for compression-sided stress fractures is protected weight bearing on the affected extremity for 4 to 6 weeks or until the pain resolves. Doctors usually avoid prescribing nonsteroidal anti-inflammatory medications (NSAIDs), which reduce inflammation, such as aspirin, Aleve®, and Advil® because these medications interfere with the inflammation that your body uses for bone healing. Tension-sided stress fractures are less likely to heal with conservative management and often require operative fixation. Treatment also consists of a progressive return-to-play protocol to avoid recurrence of the stress fracture.
 Don’t confuse a stress fracture with shin splints
Don’t confuse a stress fracture with shin splints
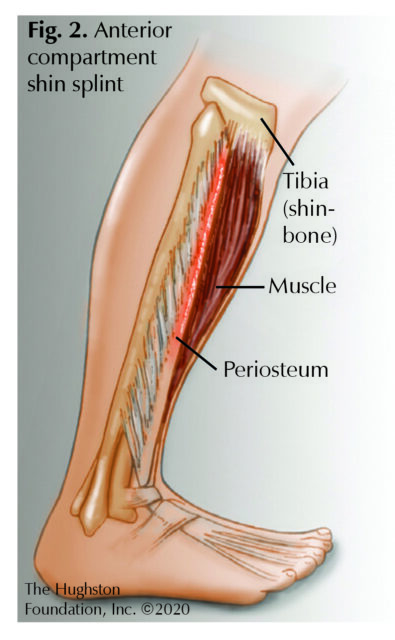
Stress fractures are commonly confused with tibial stress syndrome, also known as shin splints. Shin splints differ from stress fractures in that shin splints are an inflammation of the superficial portion of the bone called the periosteum (Fig. 2). The underlying periosteum becomes inflamed from the repetitive pull of the muscles originating in the anterior (front) or posterior (back) compartment of the lower leg. Patients most commonly report vague pain that runs along the middle to distal aspect of the tibia that increases during the start of exercise but improves with prolonged activity. Physicians often order x-rays for the patients to rule out stress fracture. Treatment for shin splints involves modifying activities until the pain subsides which can involve decreasing running distance, performing cross-training exercises, and avoiding running on hills or hard, uneven surfaces. Physicians sometimes order physical therapy as an adjunctive treatment to help with stretching and strengthening the ankle and leg muscles, tendons (tissues connecting muscle to bones), and ligaments (tissue connecting two bones).
Prevention is key
The most important factor for preventing stress fractures in young athletes and children is to recognize risk factors early. Young children should eat a healthy diet that consists of essential vitamins and protein for normal skeleton development. Children of all ages should also participate in at least 60 minutes of physical activity per day; this regular physical activity also helps to promote the development of bone strength. Additionally, coaches, parents, and athletic trainers can help identify athletes and children at risk for overuse injuries and stress fractures as well as encourage adequate recovery and rest. Furthermore, young athletes should be encouraged to seek treatment to prevent complications or need of surgical intervention from their overuse injuries.
Author: Julia Fink, DO | Columbus, Georgia
Last edited on July 27, 2022